ARVs default rate on the rise
ARVs default rate on the rise
WITH three million new HIV infections recorded in the world between 2020 and 2021, the search for a cure for HIV becomes are ever more important.
Experts believe that having 40 million people living with HIV on lifelong treatment is not sustainable in the long-term.
The recently ended United Nations General Assembly (UNGA)’s call to pool US$18 billion for the Global Fund highlighted the urgent need for a cure.
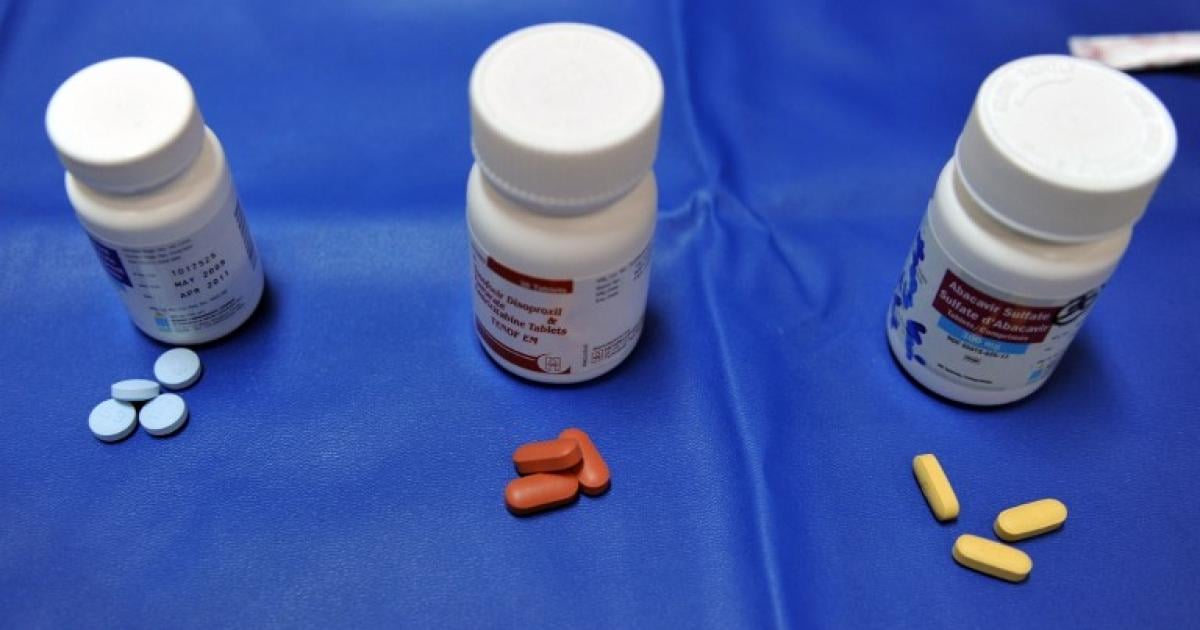
The US$18 billion is for treatment, and with antiretroviral therapy (ART) suppressing the virus only, a cure is urgently needed.
World Health Organisation (WHO) director of Global HIV, Hepatitis and Sexually Transmitted Infections Programmes, Dr Meg Doherty, said there is growing burden of new HIV infections.
“HIV prevention efforts have stalled, with 1,5 million new HIV infections in 2021 – the same as 2020.
“There were 4 000 new infections every day in 2021, with key populations (sex workers, men who have sex with men, people who inject drugs, people in prisons and transgender people) and their sexual partners accounting for 70 percent of HIV infections globally.
“Long-acting cabotegravir is a safe and highly effective HIV prevention tool, but isn’t yet available outside study settings,” she said.
Statistics as at June 2022 shows that people defaulting from ARVs first line were 49 944 and third line 489, from a total of 1,2 million people living with HIV as compared to 2019, when second line was 389.
Community Working Group on Health executive director, Mr Itai Rusike, said there has been an increase in the number of people defaulting on ARVs.
“The country is still experiencing an increased number of people who are defaulting on HIV medication.
“Even though ARVs are mostly provided free of charge at our public health institutions, there are still a number of barriers to treatment, such as transport costs, diagnostic costs and logistical challenges for Zimbabweans outside the country, especially from areas along our borders, but who rely on their ARVs supply from the country.
“The current challenges of drug abuse are also another contributing factor for defaulting on HIV treatment,” he said.
Mr Rusike said there is a need to understand reasons for defaulting in order to design improved treatment retention.
“But, what is encouraging is that Zimbabwe has almost 1,4 million people living with HIV and 1,3 million are on treatment, which is highly commendable even though we would want to have everyone living with HIV to be on treatment,” he said.
Zimbabwe Medical Awards Trust chairperson, Dr Josephat Chiripanyanga, urged people to take the virus seriously.
“There are a lot of new cases of HIV and people are also defaulting on their treatment. This is mainly because people are now reluctant, and they are saying HIV is no longer deadly as it was before,” he said.
“It has also affected us as medical practitioners in terms of managing patients with HIV and AIDS because people no longer see the importance of abstinence, the importance of taking PREP and PEP.
“We want to warn the general public that HIV is still there and people are still dying, and if you take your medication you will leave a normal and healthy life.”
Life Empowerment Support Organisation executive director, Ms Olive Mutabeni, said major defaults were witnessed during the Covid-19 lockdowns.
“Major causes of defaulting were caused by Covid-19 necessitated lockdowns.
“People were afraid of moving around to collect their medication and afraid of disclosing their status at road blocks.
“Another thing we noted during our community monitoring was the issue of test and treat, which is leaving the patients very dull because mentally they will not be prepared to accept,” she said.
She added that there is a need for the establishment of support groups that educate people on treatment literacy.
“People are still in negative mode. Treatment literacy is now limited due to limited health workers, and they are overwhelmed. Stigma and discrimination is still there, hence people are now defaulting.
“We need to revisit our palliative care, because it starts from the diagnosis process.
“More supportive care and treatment literacy and support groups,” said Ms Mutabeni.
In July, 2020, an HIV vaccine trial called Imbokodo was stopped in South Africa after it was found to be 25 percent or less effective in stopping HIV infection.
However, HIV vaccine trials continue to take place in Mexico and Brazil among the transgender community settings.
There are also trials on gene therapy in the UK and US.
A Ugandan researcher, Dr Cissy Kiyto, explained how gene therapy works.
She said the two methods, In-Vivo and Ex-Vivo, entail a therapy inside the body and the other outside in the laboratory.
“Gene therapy can be done as Ex-Vivo, outside the body, genetically modified with no need for a donor.
“The cells are taken from the patient again, so no challenges of matching donors, no fear of rejection of the cells because they belong to the patient. When modified, the cells are planted back into the bone marrow.
“With In-Vivo, an injection is given, this is the goal, we are not yet there, we will get there one day. Currently, we are working on ex-vivo. The two procedures, ex-vivo and in-vivo require no donor,” she said.